Frozen shoulder is also called adhesive capsulitis. It typically affects patients between the ages of 40 to 60 years old. It occurs in approximately 2% of the population; however, it is more common in patients with other medical conditions such as diabetes, thyroid disease and cardiac problems. Diabetes has the most common association. In patients with diabetes the incidence of frozen shoulder is high with 10-20% of this group suffering from frozen shoulder at some stage. Frozen shoulder appears to be a unique condition because it doesn’t appear to affect joints other than the shoulder and it seems to invariably resolve.
The cause of frozen shoulder and the way in which it develops is unknown. Inflammation appears to play a significant role. In many patients frozen shoulder occurs without any discernable cause, with the condition occurring spontaneously. In other patients there are precipitating factors including shoulder trauma which can be mild or severe and it can occur following an operation either to the shoulder or to another part of the body such as cardiac surgery. Frozen shoulder may also occur after prolonged immobilisation.
People with frozen shoulder experience two main symptoms. These are Pain and Stiffness.
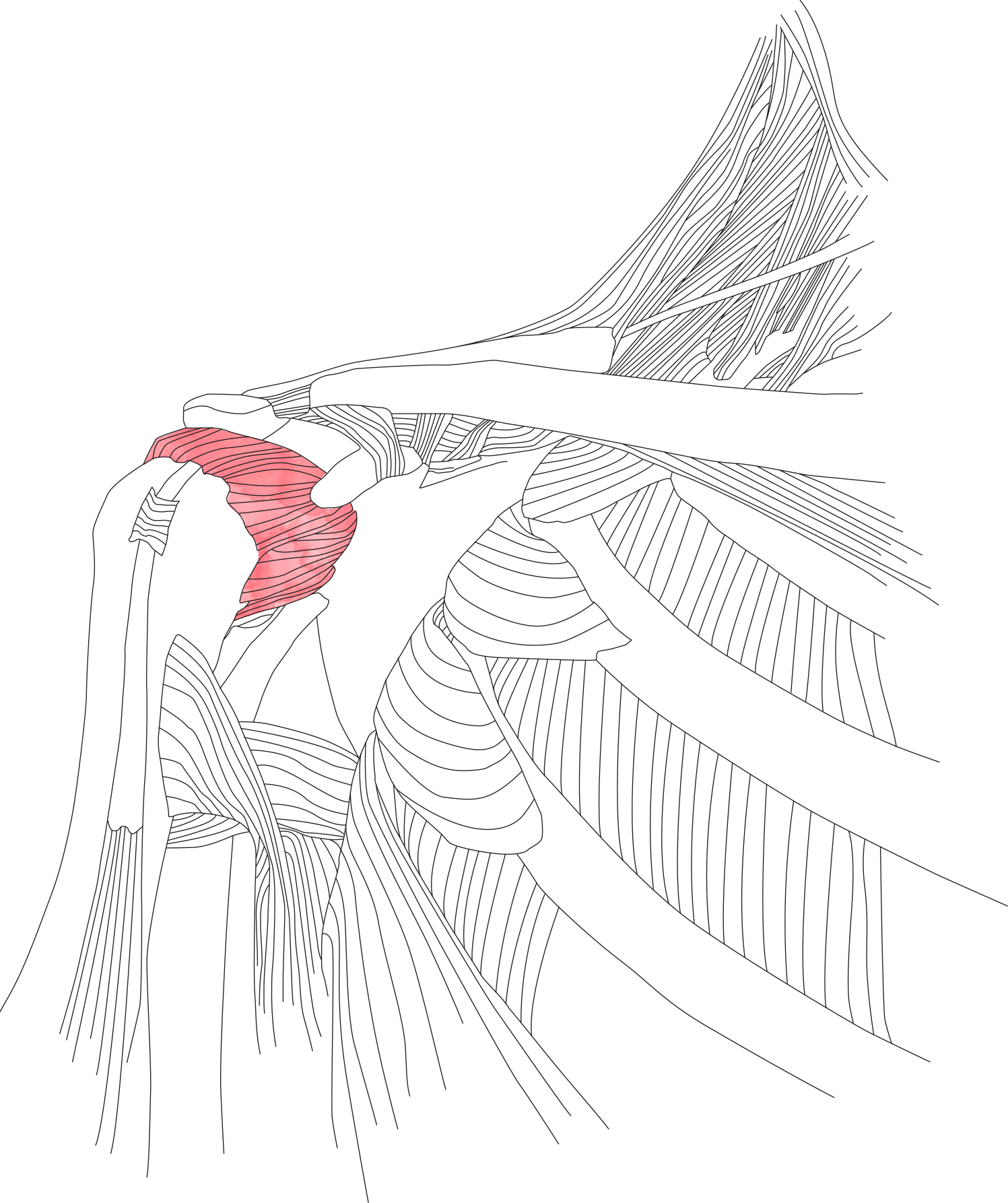
Pain is a prominent symptom of frozen shoulder. The pain tends to be a dull aching pain which is felt in the outer aspect of the shoulder and in the upper part of the arm. The pain is often worse at night time and often keeps you awake. Stiffness is also a prominent symptom and typically develops some months following the initial onset of pain. The restricted range of motion can be quite severe and incapacitating. The pain is due to inflammation in the capsule lining the shoulder joint.
Classically frozen shoulder is described as developing in three stages.
The first stage is the painful or freezing phase, this stage is characterised by the gradual onset of pain. As the pain worsens, the shoulder starts to lose its range of motion. The capsule lining the shoulder joint is highly inflammed during this phase. The capsule gradually becomes thickened and fibrous in response to the inflammation that has been affecting it. If we arthroscope the affected shoulder at this stage, the capsule of the joint will be seen to be red and inflammed.
The second stage is the stiffening or frozen phase. During this stage the pain in the shoulder gradually subsides, however the shoulder remains stiff and restricted in its range of motion. The capsule lining the shoulder joint has become substantially thickened by the inflammation that has been affecting it. The capsule is no longer a thin flexible membrane. Rather, it is now thickened and fibrous and non-pliable. The inflammation has now largely subsided. If the shoulder joint is arthroscoped during this phase, the capsule lining the shoulder will be much less inflammed than during the first stage and the capsule will be seen to be thick and fibrous. The capsule is often 5 or 6 mm thick compared to a more normal thickness of a millimetre or so.
The third stage is the thawing phase. During this stage the range of motion in the shoulder gradually increases and the discomfort continues to subside. The range of motion returns to the shoulder as the capsule of the shoulder joint remodels and returns from its thickened fibrous state to a more normal soft pliable membrane.
Frozen shoulder often takes 18 to 24 months to resolve, however it can take considerably longer in some patients. Frozen shoulder typically takes longer to resolve in people who have diabetes.
An x-ray of the shoulder is usually performed to rule out arthritis as a cause of the shoulder stiffness. A scan of the shoulder being either an ultrasound or MRI scan will often be undertaken to confirm that the rotator cuff tendons are intact. There is no single investigation that can competently diagnose frozen shoulder. Frozen shoulder is normally diagnosed on the basis of history and examination. However, an MRI scan may demonstrate thickening of the capsule of the shoulder joint and this finding may help to confirm the frozen shoulder diagnosis.
Frozen shoulder is a condition that normally resolves of its own accord. The underlying cause is unknown and consequently, there is no treatment available for the actual cause. Treatment is aimed at alleviating the symptoms of frozen shoulder, these symptoms being pain and stiffness.
A steroid injection placed into the shoulder joint is often very helpful in relieving the aching pain felt in the shoulder. The steroid injection works by decreasing the inflammation present in the shoulder joint capsule. Often a single injection can have a long-lasting effect; although the pain may be reprecipitated if there is further injury of aggravation to the shoulder. The injection will not normally make any difference to the stiffness in the affected shoulder.
When considering treatment for the reduced range of motion and stiffness that occurs it must be kept in mind that frozen shoulder resolves of its own accord even without treatment. The stiffness may be markedly improved with surgery.
Surgery will normally involve an arthroscopic release of the shoulder joint capsule. At the time of surgery Mr Peter will normally perform a manipulation of the shoulder prior to undertaking the arthroscopic release. This manipulation is undertaken following the admission of anaesthesia and prior to performing any surgical release. The shoulder is manipulated through its range of motion. This controlled manipulation of the shoulder may free the shoulder joint by creating tears in the affected capsule. In some instances, a manipulation of the shoulder joint will be all that is required. In these instances surgery can be avoided. The aim of surgery is to restore a normal range of motion to the shoulder and intra-operatively it is possible in most patients to do this.
Post-operative physiotherapy is utilised to maintain the range of motion in the shoulder. Physiotherapy is normally fairly intensive in the majority of patients to maintain range of motion following the surgical release. While the range of motion in the shoulder is normally substantially improved, it is not always completely restored following surgery.